Understanding the IVF Process from Start to Finish

If you’ve been trying to conceive and getting a “no” every month on a pregnancy test, it can be time for some reproductive assistance. IVF, or in vitro fertilization is a process that can help couples realize their dream of having a baby. Here’s what to expect in the IVF process, from the basics to a detailed step-by-step explanation to help you prepare for your IVF cycles and procedures.
What is in vitro fertilization (IVF)?
IVF stands for in vitro fertilization which means fertilization outside the body. During IVF, eggs and sperm are retrieved from the couple and combined in the lab to create embryos that are then transferred into the uterus of the mother or a gestational carrier.
IVF is a type of Assisted Reproductive Technology (ART) to help couples who may have difficulty conceiving for one or more reasons, such as fallopian tube or ovarian damage, endometriosis, previous surgical sterilization, ovulation disorders, uterine fibroids, a genetic disorder, preservation of fertility prior to surgery or cancer treatment, low sperm production or quality, or any other unexplained fertility difficulty.
What are the stages of an IVF Cycle?
The basic stages of an IVF cycle are ovarian stimulation, egg and sperm retrieval, fertilization in the lab, and embryo transfer to/implantation in the uterus. An IVF cycle lasts 2-4 weeks (about the same as an ovulation cycle) and more than one IVF cycle may be needed to become pregnant.
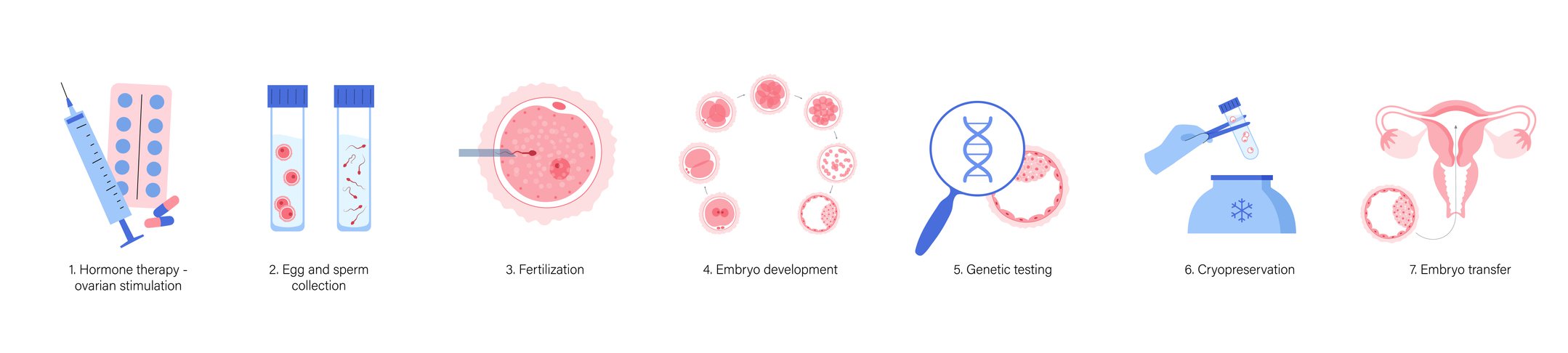
What is the IVF process step by step?
While the basic parts of an IVF cycle follow the ovulation cycle from ovarian stimulation to embryo implantation, the full IVF process from beginning to end is a bit longer, beginning with consulting a fertility specialist and preparing your body for IVF. Here is the complete IVF process step-by-step to help you understand everything that is involved with these fertility treatment procedures.
1. Consultation with your doctor
If you’ve been trying to conceive without success, it’s time to schedule an appointment for assistive reproductive technology (ART), which includes techniques such as fertility drugs, artificial insemination, and IVF. Your doctor will listen to you and partner with you to make a plan to help you on your pregnancy journey. IVF is usually a last resort after other ART methods have been attempted or to help with specific genetic diseases.
2. Fertility testing of both partners
Your doctor will do a physical examination of the uterus, cervix, ovaries and fallopian tubes to look for issues such as uterine fibroids, blocked or collapsed fallopian tubes or other structural problems. Both partners will be screened for sexually transmitted infections, and the doctor will evaluate the woman’s ovarian reserve and the man’s semen and sperm quality.
3. Tracking your ovulation and cycle
Before the IVF cycle of retrieval-fertilization-transfer can begin, you and your doctor need to be on the same page with your monthly cycle. Your doctor will likely have you use an ovulation predictor kit, track your basal temperature. They may also choose to put you on birth control pills to control your cycle, prescribe a GnRH agonist or antagonist to cause or suppress ovulation or, if you’re not getting your period, use provera (progesterone) to jumpstart it. The point of this step is to allow your IVF doctor to have control of your monthly cycle so it can sync with your IVF treatment for maximum success.
4. Baseline Bloodwork & Ultrasounds
Once you get your period, the first official day of your IVF treatment begins. On Day Two of your period, your doctor will typically order blood work to check your thyroid function and hormone levels, especially estrogen in the form of estradiol or E2. You’ll also have a transvaginal ultrasound to check for cysts or anything else that might complicate the IVF treatment.
Many cysts resolve on their own, but your doctor may decide to remove them at this point. If everything checks out, you’ll move to the next step in the IVF process.
5. Ovary Stimulation
During this stage, your doctor will give you fertility drugs to stimulate your ovaries to produce mature eggs. Typically, one egg per month matures and bursts from its follicle into the fallopian tubes from one of the ovaries (they usually trade off, left and right, from one month to the next). To improve your chances of pregnancy, your IVF doctor wants multiple eggs from both ovaries to mature and be ready to leave the follicle.
In most cases, ovary stimulation drugs are give via one to four shots every day for about a week to 10 days. During that period, your doctor will closely monitor your egg follicle development and hormone levels. That typically means blood work and ultrasounds every few days, or even daily. Your doctor may need to increase or decrease your medication dosages. Once your largest follicle is about 16 to 18 mm in size, you’re ready to move to the egg maturation step.
6. Egg Maturation
As the egg follicles grow and you have several that are 18-20mm in size, your doctor will trigger the final stage of egg maturation through an injection of human chorionic gonadotropin (hCG). This shot needs to be precisely timed so that the eggs have grown and developed enough but are not so “old” that fertilization will be difficult. You might give yourself the injection or go to the doctor’s office.
Alternately, and especially if you’ve had IVF failure or other specific fertility issues, you may receive IVM—in vitro maturation. In this case, you’ll skip the hCG shot and egg maturation step and go right to egg retrieval below. Your eggs will be forced to mature in the lab and exposed to sperm when they are ready.
7. Egg Retrieval and Sperm Collection
About 36 hours after your hCG shot, you’ll be scheduled for egg retrieval. In a minor surgical procedure, your IVF doctor will locate the mature follicles in the ovaries using a trans-vaginal ultrasound and remove those eggs using a hollow needle inserted through the cervix. The procedure usually takes less than 30 minutes, but may take up to an hour. You’ll be under mild sedation through an IV during this process.
On the same day, your partner will be asked to provide a sperm sample to be used for the next step: fertilization.
8. Fertilization
During this step, your harvested mature eggs are combined with the collected semen in a lab dish and incubator. The fertilization step takes place a few hours after egg retrieval and after the eggs have been evaluated and the most viable ones selected.
Depending on the cause of infertility, your IVF doctor will either combine eggs and semen in an incubated petri dish to allow a sperm to enter an egg through a natural insemination process or extract sperm from the semen sample and directly insert it through the egg’s membrane in a procedure called intracytoplasmic sperm injection (ICSI). Which process is used depends on the quality and motility of the sperm and other factors such as previous IVF failure.
9. Embryo Culture & Evaluation
Since multiple eggs are harvested, the fertilization process typically results in several zygotes or fertilized eggs. Over a period of about 5 days, your IVF doctor will monitor the zygotes to make sure they are growing properly and the cells are dividing as they should. They will also rate the embryos in terms of quality and viability to help select the healthiest ones for transfer to the uterus.
During this time, genetic testing will also occur if you have opted for that process or are at risk of passing on genetic diseases. Genetic testing can extend the time period from fertilization to transfer by a few days as results come in and embryos are selected.
10. Embryo Transfer
The embryo transfer procedure tends to be easier and faster than the egg retrieval procedure and typically takes place 3-5 days later, unless you’ve opted for genetic testing. Using a flexible tube inserted through your vagina and cervix, your IVF doctor will deposit one or more embryos into your uterus.
Some IVF experts recommend transferring up to 3 embryos to improve your chances of success, but this can lead to multiple births and complications for both babies and the mother. Your embryologist can select the healthiest, most viable single embryo for transfer as well. Discuss your options with your doctor and partner.
After the procedure, you’ll stay in bed until you’re discharged 4-6 hours later.
11. Two-Week Waiting Period
Now the waiting begins. Just as with an unassisted pregnancy, the fertilized egg needs to implant into the uterine lining and your body needs to begin producing pregnancy hormones to sustain the pregnancy. You may experience a small amount of light spotting, known as implantation bleeding, and you may begin experiencing early pregnancy symptoms.
12. Pregnancy Test
About two weeks after the embryo transfer, your physician will likely schedule a blood test and ultrasound to verify a pregnancy. Patients often find the two-week period to be challenging and might be tempted to test on their own. It’s important to note the levels of HCG (the pregnancy hormone) injected during your treatment may result in a false positive. It’s best to consult with your physician if you should take an at-home pregnancy test, when the time is right. If you choose to test on your own FIRST RESPONSE™ has a wide range of pregnancy test available to help confirm a pregnancy.
How long does it take to get pregnant with IVF?
Many women, especially those under the age of 35, get pregnant with IVF after their first cycle, or about 3-4 weeks from beginning the process of ovary stimulation, egg retrieval, fertilization, and embryo transfer. Repeated cycles improve your chances of success.
What is the IVF Success Rate?
IVF success rates vary depending many factors, including your age, the reason for infertility, how many times you’ve tried the procedure, and whether you’re using your own or donor eggs. According to the CDC, a woman’s age tends to be the most important factor: most recent aggregate data from 2018 shows that a woman under age 35 has about a 49% chance of having a baby after an IVF embryo transfer, using their own eggs. That percentage drops to about 27% for women over age 40 and 12% over age 43.
Visit the CDC for an interactive IVF Success Rate predictor to learn more.
As with any pregnancy, there is a chance for a miscarriage. According to the Mayo Clinic, the miscarriage rate for women using IVF with fresh embryos is about 15-25 percent, similar to the rate for women who conceive naturally. The miscarriage rate increases with maternal age for all pregnancies.
Resources
- American Pregnancy Association: https://americanpregnancy.org/getting-pregnant/infertility/in-vitro-fertilization-70966
- Mayo Clinic: https://www.mayoclinic.org/tests-procedures/in-vitro-fertilization/about/pac-20384716
- Very Well Family: https://www.verywellfamily.com/understanding-ivf-treatment-step-by-step-1960200
- Very Well Family: https://www.verywellhealth.com/ivf-5119348
- Medical News Today: https://www.medicalnewstoday.com/articles/318659
- Medline: https://medlineplus.gov/ency/article/007279.htm
- Healthline: https://www.healthline.com/health/in-vitro-fertilization-ivf
- WebMD: https://www.webmd.com/infertility-and-reproduction/guide/in-vitro-fertilization
- Arc Fertility: https://www.arcfertility.com/how-is-ivf-done-step-by-step/
- CDC ART report: https://www.cdc.gov/art/



